OVOVITRIF
Investigation of non-invasive biomarkers for the prediction of oocyte survival to vitrification.
The main objective of this project is to identify biomarkers in oocyte culture medium, follicular fluid and time-lapse imaging data to determine oocyte survival to vitrification and devitrification.
In recent years there has been an increase in the number of patients coming to the clinic for fertility preservation, whether for social, medical or other reasons. In addition, egg donation is now a common practice in assisted reproduction clinics. The technique chosen to freeze these eggs is vitrification.
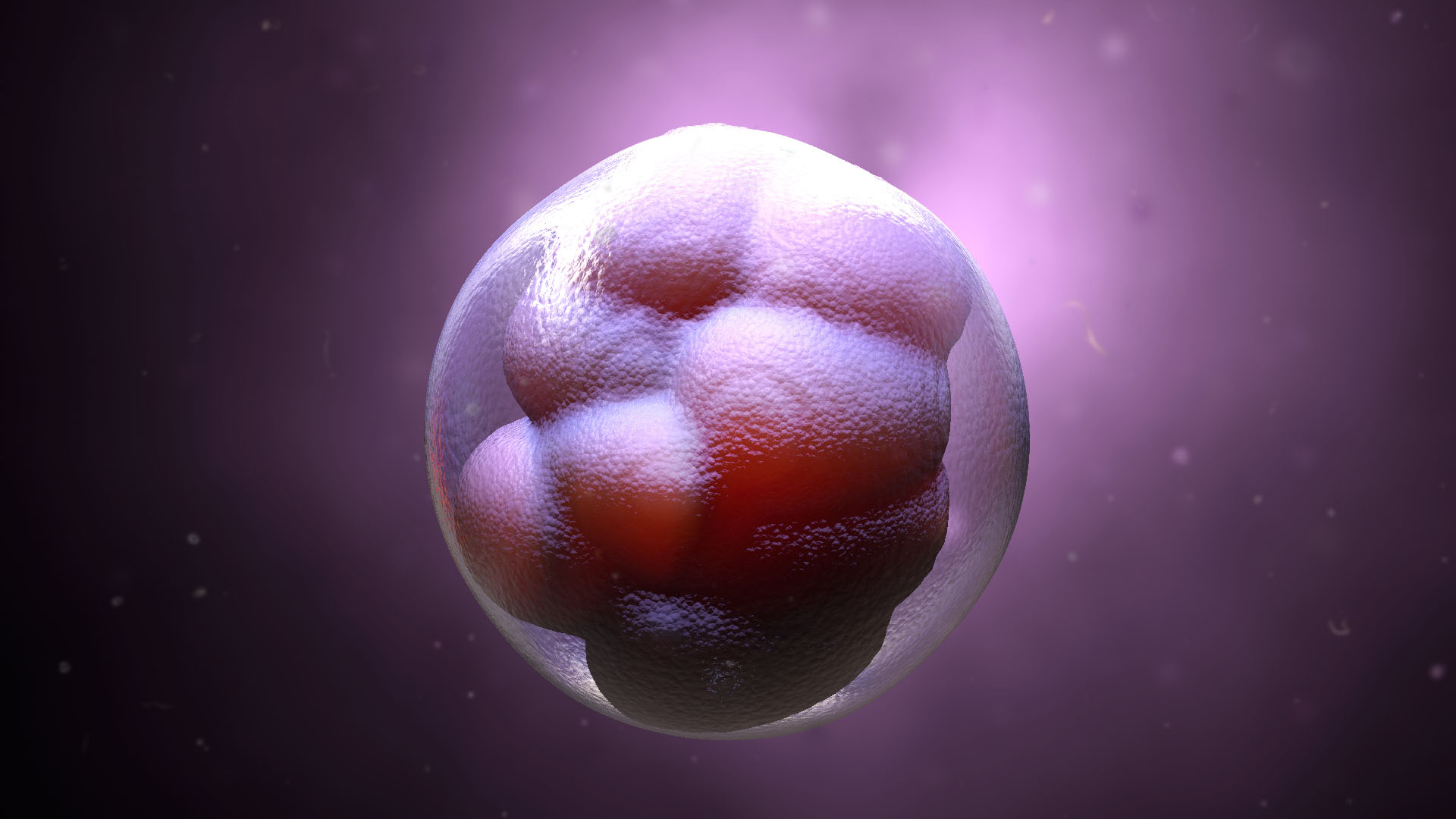
Vitrification is defined as the physical phenomenon that occurs when a solution highly concentrated in solutes is subjected to low temperatures using very high cooling rates. Its application in oocyte preservation involves the addition of a high concentration of cryoprotective agents (which replace a large part of the intracellular water), together with direct immersion of the oocyte in liquid nitrogen. In this way, the ooplasm acquires a viscous consistency with a glassy structure, which largely avoids detrimental effects on the oocyte such as dehydration and the formation of ice crystals inside the oocyte.
Oocyte banking has proven effective for oocyte donation. Vitrification is the method of choice for oocyte and embryo cryopreservation and vitrified oocyte donation is currently standard practice in many assisted reproduction centres around the world. At the IVI Valencia clinic, vitrified oocytes have been used for egg donation for 15 years.
Despite this, cryopreservation can have a negative impact on the oocyte due to the sudden changes in temperature and phase that occur in the oocyte and the osmotic stress and toxicity caused by cryoprotectants. Studies show that oocytes that survive vitrification are functionally equivalent to their fresh counterparts in terms of fertilisation, development and implantation potential. However, cryo-injury of oocytes due to chemical, mechanical and thermal causes remains a problem.
Currently, oocyte survival rates are very high, so that failure to reach 50% oocyte survival is considered a failure to survive (FSV). In some cases, there are patients with repeated failures of survival.
Predicting these cases would be of great importance for these patients, as the patient could be personally counselled and advised to undergo another cycle of stimulation if a low survival is predicted in the first cycle. In addition, in the case of donors, predicting those whose oocytes are going to present an FSV could reduce costs for the clinic by being able to reject their donation prior to vitrification. One way to do this would be to analyse the metabolomics of the oocytes prior to vitrification and to analyse the quality of each oocyte using AI techniques.
In assisted reproduction clinics, studies of sperm quality are carried out using spermograms and embryo quality using TimeLapse. However, at present, clinics do not provide information on the quality of individual oocytes, there are markers of the woman’s ovarian reserve and the degree of oocyte maturation can be studied, but their quality cannot be studied objectively for the time being.
The assessment of oocyte quality at the beginning of the cycle could provide personalised information for each patient, predict the probability of survival to vitrification, the fertilisation rate and the probability of reaching the blastocyst stage. In this way, an oocyte evaluation could even be offered to all patients on a routine basis or as an added value and help to plan the treatment of each patient in a personalised way.
For these reasons, this project aims to propose the identification of biomarkers in oocyte metabolism, in the composition of follicular fluid and with morphological markers analysed by TimeLapse to relate them to their probability of survival to vitrification. Subsequently, with the identified biomarkers, it will develop a new algorithm based on deep learning technology for the automated evaluation of oocytes prior to vitrification, which will allow personalised advice to be given to patients.
Partners